Abstract
The cytokine Fms-like tyrosine kinase 3 ligand (FL) is a key regulator of hematopoiesis. In a previous Phase 1 study testing a radioimmunotherapy regimen for relapsed/refractory acute lymphoblastic leukemia (ALL), responders showed increased soluble FL serum concentration (sFLc) after salvage regimen (Chevallier, Lancet Haematol., 2015).
This prospective monocentric study (ClinicalTrials.gov NCT02693899) aimed to assess the impact of sFLc in ALL and acute myeloid leukemia (AML) patients treated according to standard-of-care intensive first-line chemotherapy regimens. Serum samples were collected on days 1, 8, 15, 22 of induction, at days 1, 8, 15 of each intensive consolidation or day 1 of each non intensive consolidation when appropriate, frozen-stored then tested by ELISA (DY308, R&D Systems, Minneapolis, MN). The following outcomes were considered to assess the impact of sFLc: refractory status after induction (≥5% bone marrow blasts or persistent aplasia >45 days), morphologic, immunophenotypic, cytogenetic or molecular relapses, event-free (EFS) and overall survival (OS). All patients provided informed consent.
Between May 2016 and January 2018, 80 patients were included. Data were ultimately available for 16 ALL and 62 AML patients. A total of 579 samples were assayed. Analysis of the results disclosed 3 sFLc kinetic profiles during induction i) sustained increase from days 1 to 22 (FLI group), ii) increase from days 1 to 15, then decrease at day 22 (FLD group) and iii) stagnation of low levels all along (<1000 pg/mL from days 1 to 22, FLL group).
The 16 evaluable ALL patients were classified as FLI (n=2), FLD (n=7) and FLL (n=7). All reached a cytologic complete remission after induction and only 2 relapses have been documented so far in this group. No impact of sFLc kinetic profile was seen in this context.
Conversely, a significant impact of sFLc during induction (but not during consolidation) was observed in AML patients. The median age in this group was 59 years old (range: 29-71, <60 years n=33). The median follow-up for alive patients was 541 days (range: 154-787). sFLc levels were assayed in 244 samples. Twenty-six patients were classified as FLI (42%), 22 as FLD (35%) and 14 as FLL (23%). Median sFLc at days 1, 8, 15, 22 were as follows for the three groups: FLI: 2, 724, 3673, 5753 pg/mL; FLD: 6, 1229, 6019, 684 pg/mL; and FLL: 0, 60, 124, 81 pg/mL. There was no significant difference between the 3 groups regarding age, ELN 2010 risk-stratification (ELNrs), OMS classification, WBC and bone marrow blasts percentages at diagnosis.
When comparing the 3 sFLc groups, almost all refractory patients (n=6) were found in the FLL group (n=5, FLD n=1, FLI n=0, p=0.0007). Three cytologic relapses occurred in the FLI group, 7 in the FLD group (cytologic n=4, molecular n=2, immunophenotypic n=1) and 7 in the FLL group (cytologic n=4, molecular n=2, immunophenotypic n=1). There were more relapses in the FLL group (n=7/9 [78%] vs FLD n=7/21 [33%] vs FLI n=3/26 [11.5%], p=0.0009).
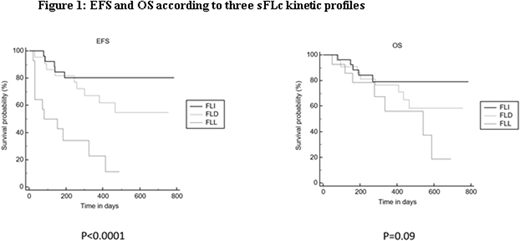
In univariate analysis, 2-year EFS and OS were significantly better for the FLI group (79.1+-8 vs FLD 54.9%+-11 vs FLL 11.4%+-10,p<0.001; and 80.4%+-8 vs FLD 58.6%+-11 vs FLL 18.6%+-10, p=0.09,respectively). There was a trend for the association of 2-year EFS (but not OS) with ELNrs (favorable:70.9%+-11, vs Int-1+Int-2:57.1%+-10 vs adverse 33%+-13,p=0.06). Stratification of the patients according to the median sFLc level at day +15 (2952pg/mL) also showed significantly different 2 year EFS at 38.2%+-9 for low levels vs 71.8%+-8 for high levels (p=0.02). The same was true for day +22 median sFLc level (1390pg/mL) at 38.9%+-9 vs 73.6%+-8 (p=0.02). Age had no impact on EFS nor OS.
In multivariate analysis considering age, ELNrs, sFLc at days 15 and 22 levels, and sFLc kinetic profile during induction, the latter remained the most powerful factor independently associated with EFS (HR: 3.62; 95%CI: 1,65-7,94, p=0,001; ELNrs: HR: 1.74; 95%CI: 0,98-3.10, p=0.05; sFLc at day+15 p=0,37; sFLc at day+22, p=0.24, age p=NS). sFLc kinetic profile was the sole factor that was also independently associated with OS (HR: 2.60; 95%CI: 1.12-6,07, p=0.02).
In conclusion, sFLc kinetic profile during induction appears to be a new powerful early prognostic parameter in AML patients. These results need to be validated on a larger cohort of patients and the mechanism by which induction sFLc levels may impact AML outcome remains to be elucidated.
Gastinne:Millennium/Takeda: Honoraria. Moreau:Abbvie: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.